Phreesia is best-known as a leader in patient intake, but after two decades in the digital health space, we’ve recognized that patients are also pivotal to solving provider challenges that extend beyond the waiting room—chiefly by taking a more active role in their care.
By supporting and improving patient activation—defined as an individual’s knowledge, skills and confidence in self-managing their health and healthcare—healthcare organizations can realize better clinical outcomes and improved financial and operational performance.
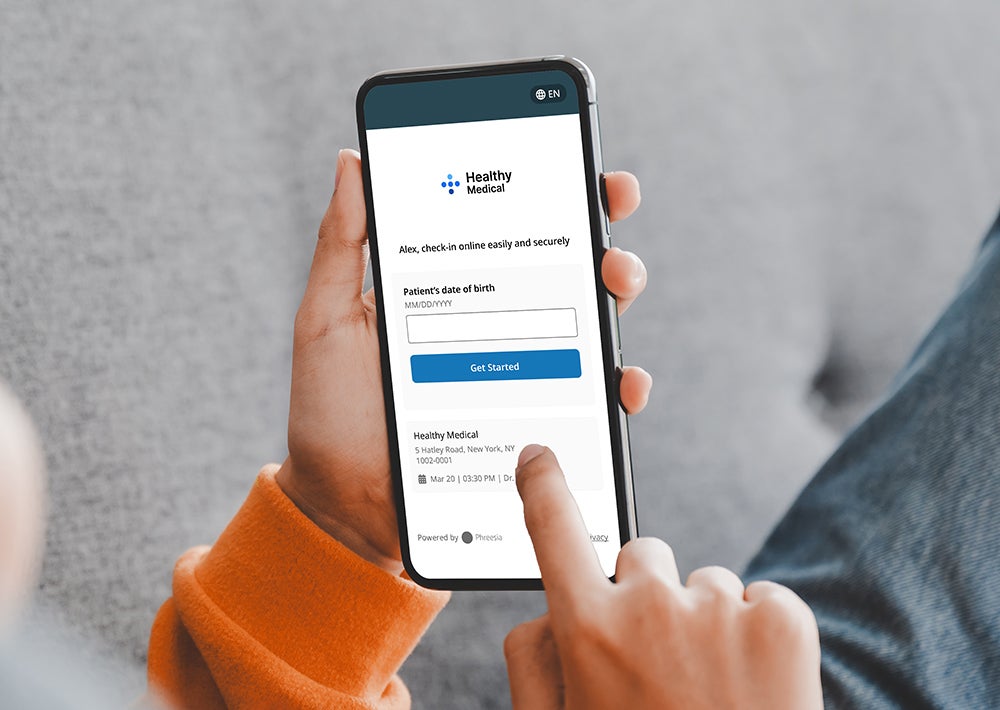
Every provider’s dream is to work at an organization where patients show up for appointments on time with check-in complete, bills paid, up to date on their preventive care and taking their medications. It’s not magic. Patients have to put in a lot of effort to make that happen, and so do staff. That’s where Phreesia comes in. Phreesia puts step-by-step support in place so that patients become better and more active managers of their care—and as a result, healthcare organizations are able to operate more efficiently and profitably.

Prioritize patient activation for business success
At Phreesia, we firmly believe in the power of patient activation to improve health outcomes, such as helping patients stay up to date on their vaccines and fill their prescriptions. But the benefits of patient activation aren’t limited to improved clinical outcomes. Phreesia works with healthcare organizations of all sizes, and we see firsthand that patient activation is the “secret sauce” that actually helps medical practices, health systems and other care settings run better. Simply put, organizations that have patients who take an active role in their care are more financially and operationally successful.
Meet patients in moments that matter
How patients manage their healthcare—how they book appointments, how they manage the costs of their care, when (or if) they fill their prescriptions, whether they set up a payment plan when offered the option—is directly related to their level of activation, and those activities have a profound impact on the health of the organizations that care for them. At Phreesia, we’ve applied what we learned about improving the intake process to building a patient-activation engine that meets patients in moments that matter. The result? Patients get the right care every step of the way, and the administrative burden on overextended staff is reduced.
Beyond check-in, there are many other key moments when patients need personal, timely, relevant and actionable information about their care. Implementing processes that make it easy for each patient to complete the right task at the right time helps activate them at critical moments in their healthcare journey.
Make it easy to book an appointment
A lot of operational waste happens during the appointment process. From finding a provider, booking an appointment or rescheduling it, to getting referrals and following up on preventive care, scheduling often produces waves of ping-ponging phone calls and waiting-on-hold misery. When patients feel overwhelmed and frustrated with the appointment-scheduling process, they may not seek the care they need. Or they may rely too heavily on overworked staff to book, rebook and remind them about upcoming visits. Phreesia eliminates that wasted time and frustration by automating scheduling and appointment processes, getting more appointments on the books—and improving financial outcomes.
An average medical practice in Phreesia’s network:
- Generates $550,000 annually through self-scheduled appointments
- Sees a 79% reduction in no-shows, resulting in an additional $200,000 in revenue per year
- Fills 2,000 additional appointments each year with Phreesia’s automated smart-scheduling tool
Increase referrals
More than one-third of patients receive referrals to specialists every year, but the process is fraught with antiquated tasks and wasted time and resources. Referrals are often sent via fax, which means that referring physicians don’t have visibility into whether their recommended appointments have actually been scheduled. Such transparency is essential for supporting patients at every step in the referrals process and ensuring that illnesses and medical conditions are diagnosed and treated before they become more serious or life-threatening.
An average specialty medical practice using Phreesia’s digital-referrals solution:
- Saves up to 21 minutes per patient referral
- Acquires 60 new patients per month
- Is 3x more likely to promptly schedule referrals
Simplify payment and insurance processes
Healthcare organizations are more financially stretched than ever before, which means that accurately verifying patients’ insurance and collecting copays and balances is critical. Phreesia helps organizations capture needed revenue—without adding to staff workloads—with automated, unlimited eligibility and benefits checks that include alerts on out-of-network and Medicare Advantage coverage. Our tools make it easier for organizations to reduce denials and have conversations with patients about their coverage upfront.
Patients want to have those conversations, too, because paying for healthcare is a major concern. In fact, 61% of patients have postponed care because they were unsure of what they might owe. Phreesia simplifies the payment process for patients by informing them about their insurance benefits and copays prior to their appointments, as well as helping them set up payment plans.
An average medical practice using Phreesia’s revenue cycle management tools:
- Collects up to $300,000 more annually using our post-visit collection tools
- Sees time-of-service collection rates increase by up to 50%, which correlates to fewer follow-up billing calls and emails
- Has 89% of its patients pay at the time of service, eliminating follow-up calls and payment delays
The bottom line
Drawing on the experience of powering 150 million patient visits each year, our team at Phreesia has learned that when patients are active participants in their care at the right moments in their healthcare journey, they become better at self-managing their health. We’ve seen that if we break the patient journey down into simple steps, we can help patients become more activated at each of those steps.
Activated patients are happier because they have helpful, relevant information at their fingertips and easy ways to get the care they need. And staff are happier because they aren’t drowning in overdue balances and uncollected copays, as well as verifying insurance, answering endless phone calls and constantly reminding patients to show up for their appointments. This dual support is vital for the financial and operational sustainability of healthcare organizations that are doing their best to keep their doors open—to save lives and to keep patients healthy.
To learn more, connect with us.





