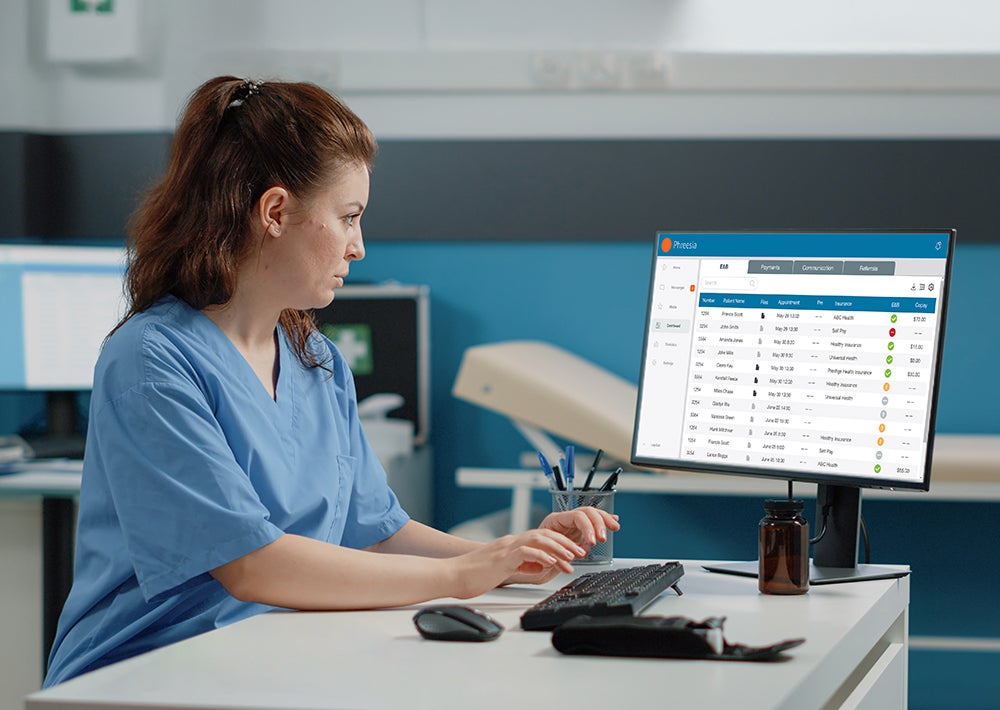
Phreesia recently submitted comments to the leadership of the Medicare program on the 2025 Medicare Advantage (MA) Capitation Rates and Part C and Part D Payment Policies. The federal government finalized those policies on April 1.
This is an important opportunity to remind policymakers of how they can best capture the interests of patients in the next round of changes to Medicare Advantage, which has rapidly become just as popular as traditional Medicare.
Read our full comments here. In this post, we summarize what we wrote to federal officials, and share why we think this moment is so important in the movement toward better patient engagement.
If you’ve followed our work in the past, you know that Phreesia is the proud steward of the Patient Activation Measure performance measure (PAM-PM), the only consensus-based entity (CBE) endorsed measure of patient activation. The performance measure is based on the PAM, a brief survey that assesses a patient’s ability to manage their own health care by measuring their knowledge, skills and confidence. More than 850 peer reviewed studies show that PAM predicts outcomes, costs and patient satisfaction with care. The evidence that increasing patient activation is critical to improving quality is so strong that the Centers for Medicare and Medicaid Services has already included the PAM-PM as part of the Merit-Based Incentive Payment System.
We believe the time has come for CMS to include the PAM-PM in the MA STARS quality rating program, and here’s why:
- A Genuine Patient Voice – Many STARS measures are oriented around process, not outcomes. When they do involve patients, they often measure the patient experience. A measure that reveals how engaged patients are in their care helps providers meet the patient where they are, and -ensures all patients get the support they need to be active participants in their care.
- Fewer, Better Quality Measures – Our entire quality measurement system needs to move away from adding more input-focused compliance measures, and towards a streamlined set of outcome-based measures that empower clinicians to deliver better care. The PAM does just that, because it is predictive of other quality measures and helps deepen the clinician/patient relationship over time.
- Addressing Specific Disparities – Without using PAM to measure activation, our healthcare system often inadvertently directs resources to higher activated patients (known as “hand raisers”). But by measuring activation using the PAM, our healthcare system can focus resources on those patients who are often less likely to seek support services. And this is vital, as patients in underserved populations often encounter more barriers to accessing and engaging in care. Through appropriate interventions, like tailored support, anyone (regardless of their starting PAM level) can become more activated and improve their health outcomes.
- Patient Activation Boosts the Other Quality Measures – The PAM-PM is an outcome measure that doesn’t overlap with or duplicate any other STARS measures. In fact, other STARS measures can also be improved by gains in patient activation. And because the PAM-PM is already included in MIPS, including it in STARS as well will align quality measures across programs.
Here’s a specific example of how the PAM-PM can make a difference. One quality measure is how frequently at-risk patients get a mammogram. With the PAM, clinicians can determine which patients need more intensive support (like in-person help) to get those appointments scheduled, and which just need simple reminders (like a digital prompt). By helping clinicians tailor their care to the individual needs of each patient, the PAM-PM is a quality measure that “lifts all boats” and could also help to reduce disparities.
Medicare Advantage has quickly grown into a program that tens of millions of Americans rely on for their health coverage and care. Patient activation is vitally important to this rapidly growing program.