The Centers for Medicare and Medicaid Services (CMS) has made numerous changes to its Merit-based Incentive Payment System (MIPS) to continue simplifying the clinician experience and enabling person-centric care in the program’s seventh year of existence.
For Year 7, clinicians may voluntarily choose to use the new MIPS Value Pathways (MVPs) framework to meet MIPS reporting requirements. CMS has also implemented changes to continue promoting outcomes-based measurement efforts, advance health equity and more effectively reward high-quality care.
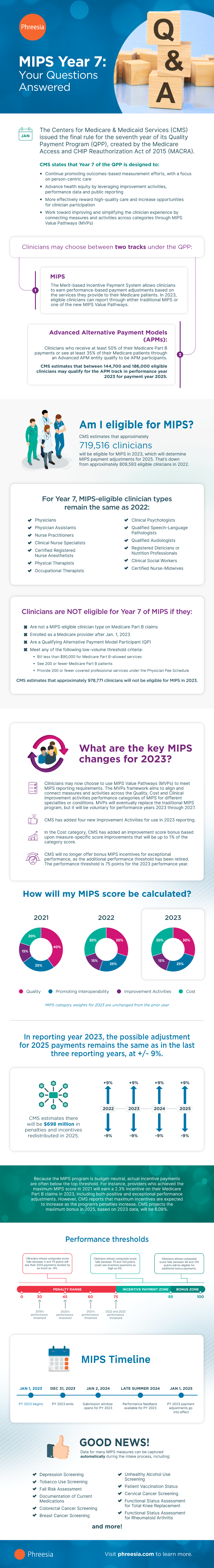
The following infographic captures important takeaways for MIPS this year, including changes to the program for 2023, eligibility criteria, a breakdown of how scores are calculated and what’s at stake for the future. You also will see that data for a variety of MIPS measures, including cervical cancer screening, fall risk assessment, documentation of current medications and many others, can be automatically captured during the intake process.
Click the image to view the full-sized infographic
MIPS Year 7: Your questions answered
The Centers for Medicare & Medicaid Services (CMS) issued the final rule for the seventh year of its Quality Payment Program (QPP), created by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA).
CMS states that Year 7 of the QPP is designed to:
- Continue promoting outcomes-based measurement efforts, with a focus on person-centric care
- Advance health equity by leveraging improvement activities, performance data and public reporting
- More effectively reward high-quality care and increase opportunities for clinician participation
- Work toward improving and simplifying the clinician experience by connecting measures and activities across categories through MIPS Value Pathways (MVPs)
Clinicians may choose between two tracks under the QPP:
- MIPS: The Merit-based Incentive Payment System allows clinicians to earn performance-based payment adjustments based on the services they provide to their Medicare patients. In 2023, eligible clinicians can report through either traditional MIPS or one of the new MIPS Value Pathways.
- Advanced Alternative Payment Models (APMs): Clinicians who receive at least 50% of their Medicare Part B payments or see at least 35% of their Medicare patients through an Advanced APM entity qualify to be APM participants.
CMS estimates that between 144,700 and 186,000 eligible clinicians may qualify for the APM track in performance year 2023 for payment year 2025.
Am I eligible for MIPS?
CMS estimates that approximately
719,516 clinicians
will be eligible for MIPS in 2023, which will determine MIPS payment adjustments for 2025. That’s down from approximately 809,593 eligible clinicians in 2022.
For Year 7, MIPS-eligible clinician types remain the same as 2022:
- Physicians
- Physician Assistants
- Nurse Practitioners
- Clinical Nurse Specialists
- Certified Registered Nurse Anesthetists
- Physical Therapists
- Occupational Therapists
- Clinical Psychologists
- Qualified Speech-Language Pathologists
- Qualified Audiologists
- Registered Dieticians or Nutrition Professionals
- Clinical Social Workers
- Certified Nurse-Midwives
Clinicians are NOT eligible for Year 7 of MIPS if they:
- Are not a MIPS-eligible clinician type on Medicare Part B claims
- Enrolled as a Medicare provider after Jan. 1, 2023
- Are a Qualifying Alternative Payment Model Participant (QP)
- Meet any of the following low-volume threshold criteria:
- Bill less than $90,000 for Medicare Part B-allowed services
- See 200 or fewer Medicare Part B patients
- Provide 200 or fewer covered professional services under the Physician Fee Schedule
CMS estimates that approximately 978,771 clinicians will not be eligible for MIPS in 2023.
What are the key MIPS changes for 2023?
- Clinicians may now choose to use MIPS Value Pathways (MVPs) to meet MIPS reporting requirements. The MVPs framework aims to align and connect measures and activities across the Quality, Cost and Clinical Improvement activities performance categories of MIPS for different specialties or conditions. MVPs will eventually replace the traditional MIPS program, but it will be voluntary for performance years 2023 through 2027.
- CMS has added four new Improvement Activities for use in 2023 reporting.
- In the Cost category, CMS has added an improvement score bonus based upon measure-specific score improvements that will be up to 1% of the category score.
- CMS will no longer offer bonus MIPS incentives for exceptional performance, as the additional performance threshold has been retired. The performance threshold is 75 points for the 2023 performance year.
How will my MIPS score be calculated?
2021
- Quality: 40%
- Promoting Interoperability: 25%
- Improvement Activities: 15%
- Cost: 20%
2022
- Quality: 30%
- Promoting Interoperability: 25%
- Improvement Activities: 15%
- Cost: 30%
2023
- Quality: 30%
- Promoting Interoperability: 25%
- Improvement Activities: 15%
- Cost: 30%
MIPS category weights for 2023 are unchanged from the prior year
In reporting year 2023, the possible adjustment for 2025 payments remains the same as in the last three reporting years, at +/- 9%.
CMS estimates there will be $698 million in penalties and incentives redistributed in 2025.
- 2022: +/- 9%
- 2023: +/- 9%
- 2024: +/- 9%
- 2025: +/- 9%
Because the MIPS program is budget-neutral, actual incentive payments are often below the top threshold. For instance, providers who achieved the maximum MIPS score in 2021 will earn a 2.3% incentive on their Medicare Part B claims in 2023, including both positive and exceptional performance adjustments. However, CMS reports that maximum incentives are expected to increase as the program’s penalties increase. CMS projects the maximum bonus in 2025, based on 2023 data, will be 6.09%.
Performance thresholds
Clinicians whose composite score falls between 0 and 75 points will see their 2025 payments docked by as much as -9%.
Clinicians whose composite score falls between 75 and 100 points could see incentive payments as high as 9%.
- 2019 performance threshold: 30 points
- 2020 performance threshold: 45 points
- 2021 performance threshold: 60 points
- 2022 and 2023 performance threshold: 75 points
MIPS Timeline
JAN 1, 2023: PY 2023 begins
DEC 31, 2023: PY 2023 ends
JAN 2, 2024: Submission window opens for PY 2023
LATE SUMMER 2024: Performance feedback available for PY 2023
JAN 1, 2025: PY 2023 payment adjustments go into effect
GOOD NEWS!
Data for many MIPS measures can be captured automatically during the intake process, including:
- Depression Screening
- Tobacco Use Screening
- Fall Risk Assessment
- Documentation of Current Medications
- Colorectal Cancer Screening
- Breast Cancer Screening
- Unhealthy Alcohol Use Screening
- Patient Vaccination Status
- Cervical Cancer Screening
- Functional Status Assessment for Total Knee Replacement
- Functional Status Assessment for Rheumatoid Arthritis
and more!
Visit phreesia.com to learn more.